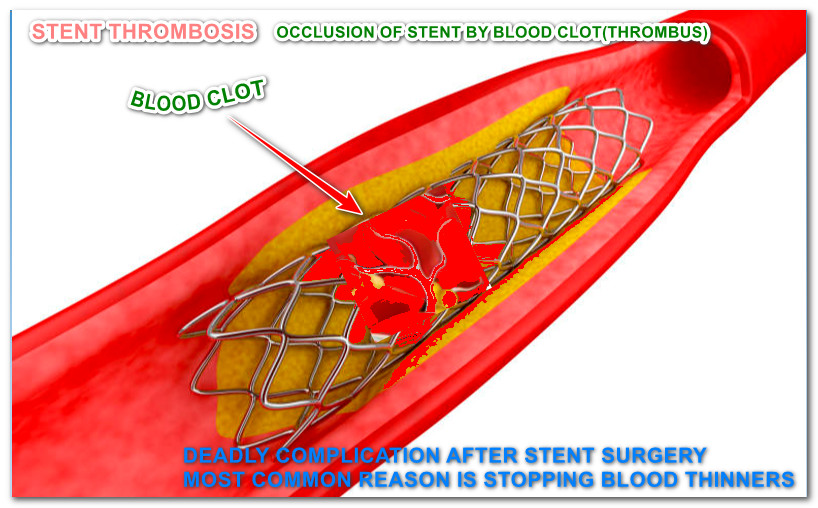
What is stent thrombosis?
Stent surgery is performed to open the narrowed vessel of the heart. It is done to alleviate symptoms and reduce death. Few individuals experience sudden occlusion of their heart stents due to the development of blood clots inside them. This is called stent thrombosis. Here, we are discussing the incidence of stent thrombosis and the causes for it.
Stent thrombosis is a major complication
Stent thrombosis is not a minor complication. It is one of the serious complications that can happen after stent surgery. It can lead to even a major heart attack and death.
When can stent thrombosis occur?
Stent thrombosis can occur within 24 hours or as late as one year or more after stent placement. Most cases of stent thrombosis, occur within the first 30 days after placement. Stent thrombosis is not uncommon.
What is the incidence of stent thrombosis?
The rate of stent thrombosis at one year is about one percent and thereafter risk decreases. The yearly rate following one year is about 0.2 percent per year.
Importance of good compliance with blood thinners
There are various risk factors for stent thrombosis. The single most important factor for stent thrombosis is the cessation of blood thinner usage. There are various causes for the discontinuation of blood thinner by the patient.
Various regions for discontinuation of blood thinners by the patients.
1. Lack of Affordability is one of the major reasons, especially in the poor.
2. Lack of awareness among the patients about blood thinners’ importance is the other reason.
3. Few people stop them when they develop side effects from the blood thinners
4. During other surgeries, heart patients are often asked to stop their blood thinner for a few days by their treating doctors.
5. Few doctors lack the knowledge regarding the optimum duration of the blood thinners, they may ask their patients to stop blood thinner inadvertently.
Who are at risk of stent thrombosis?
Stent thrombosis risk is not uniform among all the patients. Few factors put some patients at high risk of stent thrombosis. Here, we are mentioning a few important risk factors for stent thrombosis.
Following patients are at higher risk of stent thrombosis
1. Patients with diabetes mellitus or DM
2. Patients with kidney disease (CKD)
3. Patients who continue smoking
4. Patients with a weak heart (low ejection fraction) or congestive heart failure
5. Patients with Malignancy or cancer
6. Patients who underwent emergent DES stent placement.
7. Patients with Greater heart stent length(stent size more than 28 mm)
8. Patients with narrow heart stent (stent size less than 2.5 mm)
9. Patients who underwent heart stenting surgery for bifurcation lesions
10. Patients with multiple heart stents (3 or more heart stents)
11. Patients with overlap heart stents (two adjacent stents overlapping with each other)
12. Patients who underwent heart stenting surgery with first-generation stent (older generation stents)
13. Patients on dialysis
Some procedural factors are also responsible for the increased risk of stent thrombosis. Incomplete stent expansion during stent deployment is one of the causes of
stent thrombosis. Dissection after stent placement is one more reason. Stenting in severely calcified lesions carries a high risk of stent thrombosis than stenting in non-calcified vessels.
It is recommended for every heart patient who underwent stent surgery to strictly continue their blood thinners as advised by your cardiologist (heart doctor) without fail. This is the only way to reduce stent thrombosis.